Isolation to Inclusion: gathering a community for Hope and Healing

As I write this, we’re simultaneously recovering from, reflecting on and (we’ll admit it) giving ourselves a little bit of a pat on the back after the success of our recent event, ‘Isolation to Inclusion: the Journey to Hope and Healing’.
The event drew on momentum building in Wales, boosted by the Welsh Government’s Mental Health and Suicide Prevention Strategy, towards approaches to mental health that recognise the importance of community in helping each of us have the conditions for good mental health.
People, opportunity, connection – they all help us to heal. And the fact that this is built into the fabric of the Strategy shows a clear step away from older, individualised ways of thinking that seeks to treat people separately from their circumstances.
On the ground, however, the day-to-day reality is that this kind of work can be really hard. Moving into new ways of working and out of established practices can be challenging, even when there’s a strong will to change.
The event: gathering the stories in one space
As the saying goes, a problem shared is a problem halved, or at least reduced. It’s when we gather together that we can share ideas and keep that momentum growing.
That’s why we wanted to share a group of our projects that are proactively challenging that individualised approach to mental health and focusing instead on collective and community-led responses (you find out more about these projects here.) We wanted, too, to invite people to get involved in our new Hope and Healing project (more about that later).
Our aim with Isolation to Inclusion was to share some examples of how we have done this work, to build excitement about the possibilities, to be honest about how hard it can be, and to share what we’ve learnt so far. We also wanted to hear how others are doing this work – we’re learning as we go, so we’re grateful for the knowledge of those who are also on this journey (and often ahead of us), and for all the examples, advice and suggestions we find.
At its heart, this work is about relationships and participation, so we wanted to create an event rooted in connection and which created spaces for different kinds of engagement.
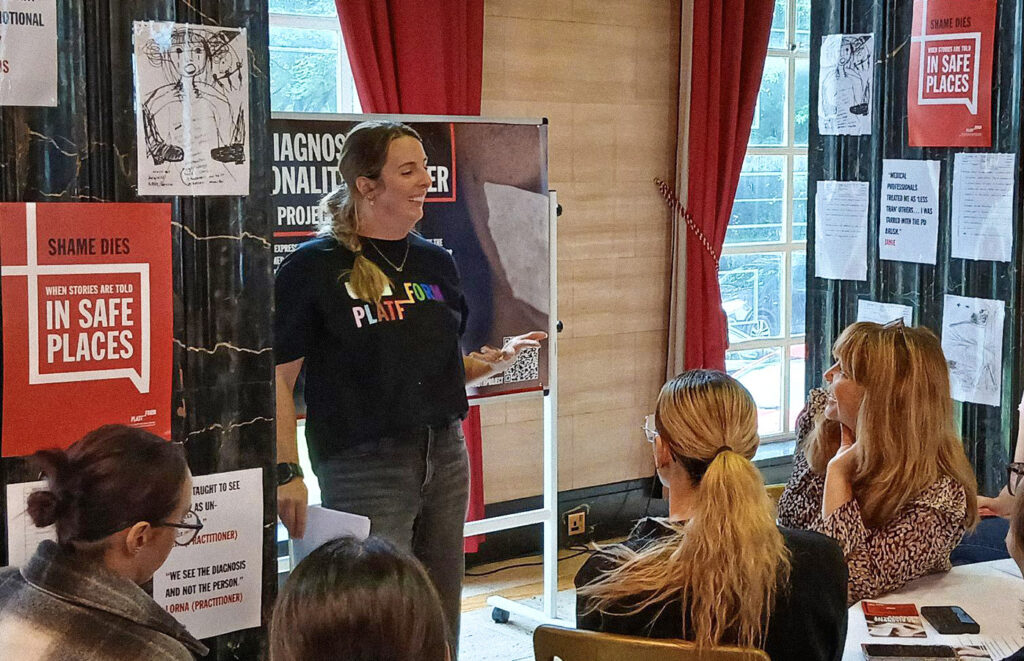
We ditched presentations (mostly) and instead opted for a carousel of mini-sessions that included an open exhibition, a conversation with parents about what learning about trauma as a community has meant for them, recreating a coffee morning and revealing, with the help of ultra-violet pens, the unheard stories of distress hidden behind medical notes.
The people who came: gathering a community
Typically, when you’re planning an event, you identify your target audience, i.e. ‘who do we want to hear about this work?’ . Our first thoughts focused on those who have obvious power in the system. But when we dug deeper, we found ourselves thinking just as much about ‘who do we want to hear from about this work?’
We realised we were thinking less about engaging an audience and more about building a community. We wanted the event to be part of a conversation about community-led responses to mental health, to create connections between people who are working in this way – and those who want to but are perhaps stifled by current workplaces, or are figuring out how to start.
So we changed tack, and decided the event was for ‘anyone and everyone who cares about doing this work.’
Away from the quiet corners
That’s because these conversations and ways of working affect us all, and we need to make sure that they don’t remain in quiet corners that only have space for policy-makers and NHS leaders. Conversations about the roots of distress and the things we need around us to heal need to be open conversations that draw on different kinds of knowledge, experience and expertise.
In the end, the people who joined us at Isolation to Inclusion came from health boards, national bodies, small and large charities, local community groups, and as staff, volunteers and citizens. For us, it was a perfect mix.
This community-building is at the heart of where we are now with our new five-year Hope and Healing project, made possible thanks to the Lottery Community Fund. I’ve been working on the project for three months and digging deeper to really understand where we are is key – not just in Platfform and with our project partners, but the wider context in which we’re working.
This involves a lot of talking, a lot of reading and thinking, but mainly a lot of listening: all those things that are fundamental but don’t always feel like ‘real work’ in a world that (perhaps over-) values a certain king of action.
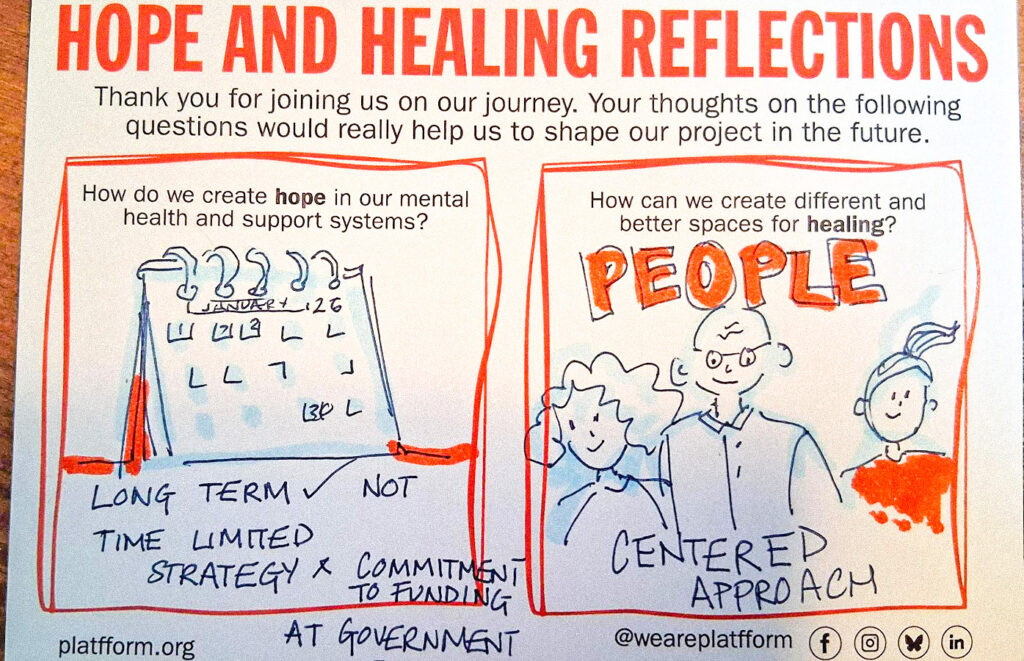
We did a lot of talking and a lot of listening at our event – as did everyone else in the room. We finished by asking everyone two questions: How do we create HOPE in our mental health and support systems? And ‘How do we create different and better spaces for HEALING?’
Their responses are worth sharing.
What we heard when we asked: “How do we create HOPE in our mental health and support systems?”
These responses were emphatically focused on relational approaches and connection: out of 62 comments, only two were operational (a small number might have gone in either category, depending on how they were implemented in practice).
Two key themes characterised responses about creating hope: listening, being heard and sharing stories and sharing power. These two themes often overlapped, emphasising the connection between being heard with having power. People emphasised how important it is to listen deeply to the people we’re supporting, which requires spaces where people can be heard and feel validated.
Being heard can lead to building the confidence to make changes. People shared ideas for qualities of effective listening e.g. open, non-judgemental, empathetic, ‘human to human’ and ‘curiosity’. People reminded us that professionals need to be listened to and heard, too, particularly in the context of burnout and moral injury. We’ve said it before and we’ll say it again: being seen and heard is a mental health intervention.
To create hope, we need to share “stories of hope” and ”voices of positivity about what is possible”. Responses point to stories as vehicles for change that enable us to imagine different futures: we need different stories, and different conversation.
People also told us that these stories need to be shared across the system, including with funders. We need to create shared spaces for people across the system to come together e.g. “Co-create spaces for system “owners” to listen and come with curiosity”.
Sharing hope means sharing power
Rebalancing and sharing power also really mattered to people. Responses talked explicitly about being less hierarchical, more radical and ‘bottom up’, including being led by people with lived experience. There was a clear connection between being having power and having hope: “it’s hard to feel hope if you have no control”.
Changing the power dynamic between professionals and those who use services is also key if we’re to create hope: redressing an imbalance in the value given to professional and patient perspectives, the need for ‘human to human’ interactions, and increasing the number of professionals with lived experience.
These all point to a recalibration of the divide between people delivering services and people accessing them; a move towards greater equity and connection. After all, people who deliver services are much more than their professional role, and will almost certainly know people who experience difficulties or experiences challenges themselves at some point in their lives.
Some responses suggested that this divide is in some ways outdated: “get them [professionals] to share their voices, too (They aren’t that different to the voices of service users)”.
If knowledge is power, then unequal access to knowledge creates a power imbalance (also known as epistemic injustice). Support and practice are based on theories and models of change – so we need to ensure that these are made accessible, and that they can be easily understood by everyone. This includes making sure that events like Isolation to Inclusion are available to people accessing support, as one respondent reminded us. And, at every point, we need to be aware of, and address, our own assumptions and biases.
We need to put hope at the heart of our work and be “willing to be the person to hold the hope whilst others can’t”.
What we heard when we asked: How can we create different and better spaces for HEALING?
Some people shared ideas about the kind of physical spaces that could support healing: moving out of medical spaces into “non-clinical spaces, going into the community and ‘reaching people where they are”, and using existing community assets and spaces. Nature, outdoor spaces, play and creativity all matter, too.
There were some reflections, too, on the need for spaces themselves to heal: “Maybe we don’t need to CREATE these spaces but acknowledge they are already there but we have disconnected from them and no longer look after them. How do we heal our spaces?”
Spaces for healing need to be safe, non-judgemental comfortable and open; they need to be quiet, flexible, neurodivergent-friendly, warm, trauma-informed. One person was keen to point out that these qualities need to extend beyond those healing spaces into the wider world: “Keep creating warm comfortable spaces where judgement is left at the door and not picked back up on the way out”.
People also thought deeply about the ‘how’ and ways of doing. The majority of responses engaged with the idea of ‘doing with’ in different ways, and of closer collaboration between people who deliver and people who use services: we need to go to where people are, ask them what they want, and avoid assumptions e.g. ask what ‘safe’ actually means for a community.
Again, sharing power matters, including rebalancing power away from medical professionals, involving people using services, co-production and community-led design.
Keeping it going
For me, two key messages rise up from the rich and thoughtful detail of these responses: ‘listen deeply’, and ‘less them, more us’.
These are two principles that we’ll challenge ourselves to hold on to as we develop our Hope and Healing project and community. If you’d like to be part of that community and help us continue the conversation, regardless of what it says on your lanyard or whether you even have a lanyard, then please get in touch.